What Bipolar Disorder Screening Involves
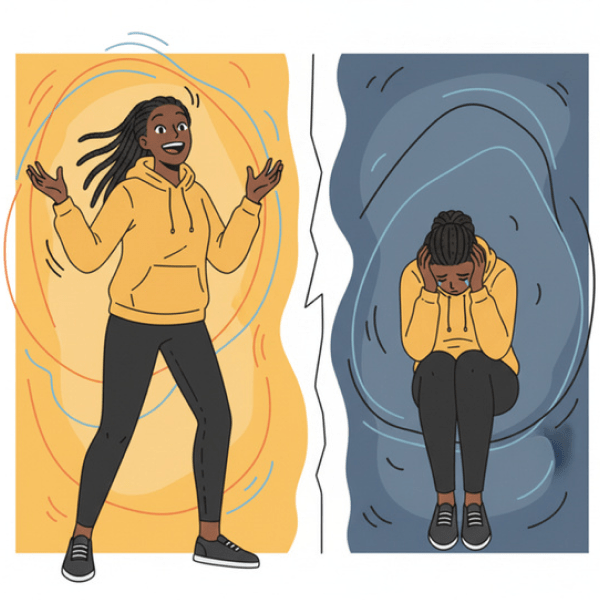
Mood storms, cycles of elevated energy, and stretches of crushing fatigue can be confusing, especially when they disrupt work, relationships, and sleep. Early self-reflection helps people notice patterns that might otherwise blend into daily life. The right information also reduces stigma by explaining how brain-based conditions manifest, fluctuate, and respond to care. When readers learn what a screening can and cannot do, they gain the confidence to start a thoughtful conversation with a clinician and avoid misinterpretation.

Many people begin with structured checklists to organize complex experiences, and tools such as a bipolar test can help turn vague feelings into specific examples that are easier to discuss. Instead of guessing, respondents review concrete prompts about changes in activity, decision-making, and sleep that track with common symptom clusters. This kind of guided reflection builds a bridge between lived experience and the language of clinical evaluation, which lowers the barrier to seeking professional input.
Screening Vs. Diagnosis
In clinical intake, providers might include a bipolar disorder test alongside a full medical and psychiatric history to establish a baseline for follow-up. The purpose is to screen, not to diagnose, and to flag topics that deserve a deeper look during a comprehensive appointment. Primary care teams sometimes share a bipolar disorder screening questionnaire prior to visits to save time and improve the quality of the interview.

A Closer Look at How Bipolar Assessment Works
Digital tools frequently include a bipolar quiz that asks about energy surges, racing thoughts, decreased need for sleep, and risk-taking behaviors in a neutral, nonjudgmental tone. Paper-based options may resemble a bipolar questionnaire with frequency and severity ratings that make subtle shifts visible across time. Interpretation is strongest when it is folded into a larger bipolar assessment conducted by a qualified clinician who can separate overlapping issues such as ADHD, thyroid problems, substance use, and trauma responses.

Comparing Popular Tools and What They Measure
People often appreciate clarity on how different screeners vary in length, focus, and purpose, because that makes it easier to pick the right starting point. Some platforms host a free online bipolar test intended to give a quick read on whether certain experiences merit a deeper look with a practitioner. Others bundle educational content with their forms so readers can connect questionnaire items to real-world examples like impulsive spending, erratic sleep, or sudden bursts of productivity.
| Tool Type | Approximate Time | What It Highlights |
|---|---|---|
| Ultra-brief screener | 2–4 minutes | Initial red flags and whether to pursue a full evaluation |
| Standard self-check | 5–10 minutes | Mood elevation, depression cycles, sleep changes, and impulsivity |
| Extended inventory | 12–20 minutes | Pattern differentiation, episode duration, and functional impact |
| Clinician-administered scale | 15–30 minutes | Structured interview with probing for medical and contextual factors |
Some organizations share a free bipolar quiz to lower barriers for those who worry about cost or privacy, and that approachable format can encourage people to track symptoms over time. Educational sites may also provide a bipolar disorder quiz embedded within a broader mood-disorders hub, which helps readers compare indicators of hypomania, mania, mixed features, and depressive episodes in a single place. When selecting a resource, it is wise to favor instruments linked to published research or professional societies.
In families navigating complex behavior changes, a clinician might use a childhood bipolar disorder questionnaire to organize multi-informant reports into a coherent picture that supports careful follow-up. Adults exploring their own patterns sometimes wonder what a quick self-check can reveal, and some turn to an am I bipolar quiz during periods of heightened worry to make sense of dramatic swings. A primary-care practice may also share a bipolar screening questionnaire when patients report uncharacteristic risk-taking or reduced need for sleep amid elevated mood, because that can flag the need for specialty referral.

Practical Steps After Bipolar Disorder Screening
Thoughtful screening can shorten the time to relief by motivating timely appointments and clearer conversations about goals. Personality-focused instruments occasionally appear alongside educational articles, and readers may encounter a bipolar personality test labeled as fun or exploratory, though it is important to treat such content as informational rather than clinical. For those intensely struggling with low mood and slowed activity, a bipolar depression test may illuminate features like atypical sleep patterns or mixed states that deserve prompt attention in care planning.

Practical follow-through matters as much as the initial score, including documentation, symptom journaling, and collaborative decision-making with a qualified clinician. Telehealth directories sometimes advertise services that suggest an online bipolar diagnosis, yet a definitive determination requires a comprehensive medical and psychiatric evaluation that includes history, ruling out mimicking conditions, and functional assessment. Used ethically, screeners empower individuals to speak up earlier, reduce uncertainty, and engage in evidence-based conversations about therapy, medication, lifestyle strategies, and support networks.
Frequently Asked Questions
The Latest News



Please Note
This website (bipolarassessment.net) is not an official representative, creator or developer of this application, or product. All the copyrighted materials belong to their respective owners. All the content on this website is used for educational and informative purposes only.
